ref) 2023 EULAR recommendations for SLE
遅ればせながらEULAR推奨2023を訳していきます。たまにはdeepLを使わずに(笑)
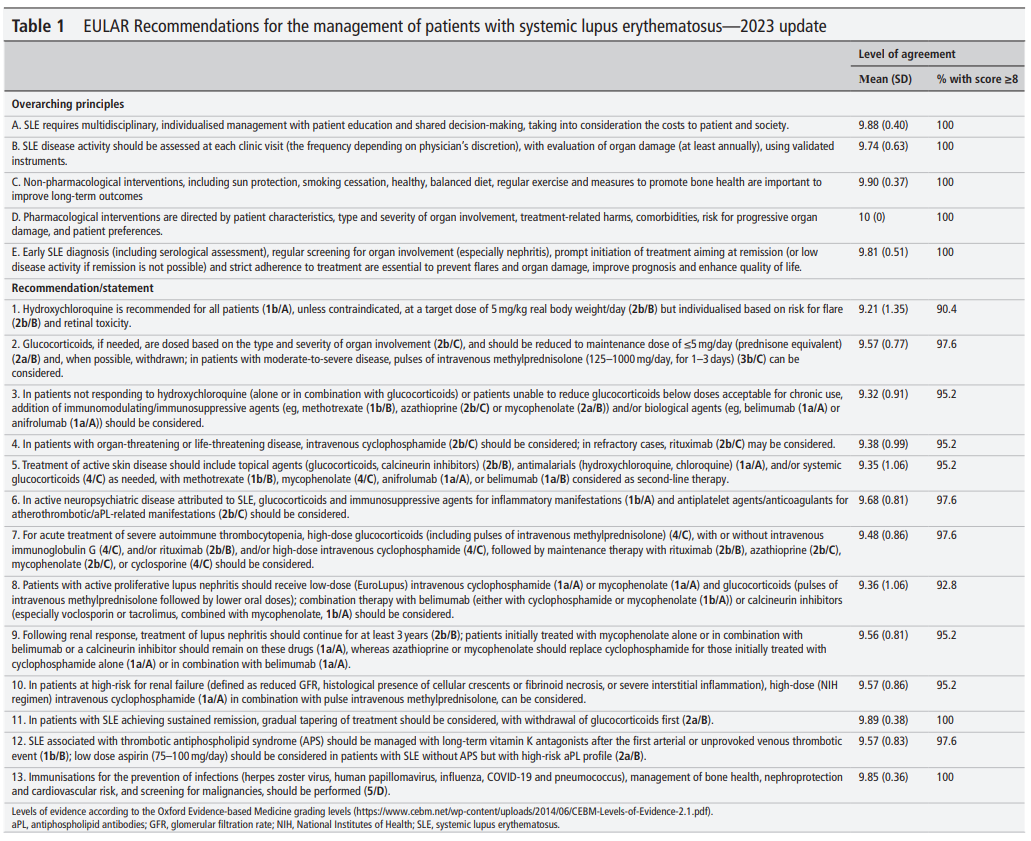
Overarching principles全般的指針
The overarching principles contain general information on the management of SLE, reflect common sense and are not accompanied by a respective level of evidence. They are nevertheless important to set an overall framework for the approach to a patient with SLE and highlight the role of physician–patient interaction. The overarching principles were voted as a group of principles (ie, not individually) and agreement was 100%.全般的指針はSLE管理の一般的な情報を含み、常識を反映し、各々のエビデンスレベルは伴わない。しかし全般的指針はSLE患者へのアプローチの全体的な枠組みを設定するために重要であり、医師と患者の関係の役割に焦点を当てる。全般的指針は指針の群として投票され(個々ではなく)、100%の賛成を得た。
- SLE requires multidisciplinary, individualised management with patient education and shared decision-making, taking into consideration the costs to patient and society.
While rheumatologists are the specialists who should primarily care for patients with SLE, the multisystem nature of the disease often mandates the involvement of other disciplines (eg, nephrologists, dermatologists etc), and treatment decisions should be individualised considering patient preferences and patient education. Comparative costs of different treatments should be weighed against the cost of illness and the societal impact of SLE, in terms of social and work participation. Mean (SD) LoA was 9.88 (0.40).
- SLE disease activity should be assessed at each clinic visit (the frequency depending on physician’s discretion), with evaluation of organ damage (at least annually), using validated instruments.SLEの疾患活動性を医師の裁量に基づく頻度に基づく受診のたびに評価し、年に1回は臓器ダメージを評価する。妥当性のある評価法を用いて。
Task Force members agreed on the need to formally assess lupus disease activity at each visit for the need of therapy adaptation. The phrasing ‘frequency depending on physician’s discretion’ was decided following deliberations, in which it became clear that optimal frequency of patient visits may vary, from a few days in a patient with active LN to up to 6 months in patients with long-standing quiescent disease; thus, judgement of the treating physician cannot be substituted by a fixed range of intervals. The most frequently used validated instruments for measuring disease activity are the various versions of the SLE Disease Activity Index (SELENA-SLEDAI or SLEDAI-2K) and the British Isles Lupus Assessment Group (BILAG). Annual assessment of irreversible damage is important because damage accrual has significant prognostic value. 委員会メンバーは治療の適応の必要性のためのすべての診察においてSLEの疾患活動性を正式に評価する必要性があることに同意した。「医師の裁量に基づく頻度」でという記載は以下の2点を考慮に入れて決められた;理想的な受診の頻度が、活動性LNのように数日に1回という頻度から長期安定の病状における6か月に1回まで、といった具合に様々であることは明白であること;そのために治療医の判断は定期的な受診の間隔にとって代わられるものではないこと。もっともよく使用される疾患活動性の指標はSLEDAIの様々なバージョン(SELENA-SLEDAI or SLEDAI-2K)とBILAG。不可逆的なダメージを毎年評価することはダメージの蓄積こそ有意な予後不良因子であるためである。Mean (SD) LoA for this principle was 9.74 (0.63).
- Non-pharmacological interventions, including sun protection, smoking cessation, healthy, balanced diet, regular exercise and measures to promote bone health are important to improve long-term outcomes.薬物以外の介入、日光を避ける事、禁煙、健康的でバランスの良い食事、規則的な運動、骨の健康を促進する方法が長期的なアウトカムを改善するために
These interventions are not specific to SLE and pertain also to the general population, although patients with lupus should particularly avoid sun exposure due to the characteristic photosensitivity of the disease. The importance of smoking cessation should be emphasised, as smoking may also interfere with the efficacy of antimalarials14 and biologics (belimumab)15 among its other detrimental sequelae. Importantly, a dedicated set of EULAR recommendations on non-pharmacological management of SLE and systemic sclerosis were published recently; the reader is referred there for more relevant information.16 これらの介入はSLEに限ったことではなく、一般人口にも通ずる。ただしSLE患者ではその日光過敏症という特徴のため特に日光暴露を避けなければならないが。禁煙の重要性は強調されるべき。喫煙はその有害な後遺症の中でも抗マラリア薬とベリムマブの効果に邪魔をするため。大切なことはSLEと強皮症の非薬物的管理に関する専門的なEULAR推奨が最近出版された;より詳細な情報はそちらを参照されたい。Mean (SD) LoA was 9.90 (0.37).
- Pharmacological interventions are directed by patient characteristics, type and severity of organ involvement, treatment-related harms, comorbidities, risk for progressive organ damage and patient preferences.薬物療法は患者の特徴、臓器障害のタイプと重症度、治療関連の有害事象、併存疾患、進行性臓器ダメージのリスク、および患者の好みによって指示される。
The phenotypic heterogeneity and variable severity of organ involvement, as well as differential response to drugs based on patient characteristics, mandate an individualised approach. Pharmacological treatment of lupus may range from hydroxychloroquine (HCQ) monotherapy for patients with mild skin and/or joint symptoms, to highly potent immunosuppressive medications like high-dose glucocorticoids (GC) and cyclophosphamide (CYC) in patients with organ-threatening or life-threatening disease. When choosing therapy, immutable characteristics, such as race and ethnicity, as well as socioeconomic determinants and access to different drugs should be taken into account. For example, black patients with LN may be more responsive to mycophenolate than CYC.17 Patient research partners in the Task Force highlighted the importance of patient preferences in the treatment decisions, which form the basis of shared decision-making. This principle received the highest mean LoA, mean (SD) 10 (0), indicating complete agreement of all individual panellists.表現型の不均一性と臓器障害の多様な重症度は患者の特徴に基づく、異なる薬物への反応性はもちろん、個々の患者に応じたアプローチが必要である。軽症の皮膚and/or関節症状を有する患者に対するHCQ単剤による治療から臓器や生命を脅かす合併症を有する患者に対する高用量GCとCYCのような非常に強力な免疫抑制療法まで。治療を選択するとき人種と民族ような変わりようのない患者の特徴は、社会経済的な決定因子と異なる治療薬への利用可能性に加えて考慮に入れられるべき。例えばLNを有する黒人はCYCよりもMycophenolateにより反応しやすいかもしれない。専門委員会は治療決定における患者の好みの重要性を強調した。これはSDMの基本である。この原則は最も高いLoA10(SD0)に値した。つまりパネリストのすべてが完全な同意を示したのだ。
- Early SLE diagnosis (including serological assessment), regular screening for organ involvement (especially nephritis), prompt initiation of treatment aiming at remission (or low disease activity if this is not possible), and strict adherence to treatment are essential to prevent flares and organ damage, improve prognosis and enhance quality of life. SLEの早期診断(血清学的評価を含む)、定期的な臓器障害のスクリーニング(とくに腎炎)、寛解に向けた早期の治療開始(あるいは寛解が難しければ低疾患活動性)、そして治療への厳格なアドヒアランスが再燃と臓器ダメージを防ぎ、予後を改善しQOLを高めるために必須である。
The final overarching principle highlights four pillars in the management of SLE: (1) need for early diagnosis, because despite increased awareness in combination with the new, more sensitive classification criteria,18 recent studies support that patients with SLE still face diagnostic delay (median 2 years from onset of symptoms)19 20; (2) vigilant monitoring for new organ involvement, mainly LN, especially during the first years of the disease, but also thereafter. This need for increased awareness for signs of new-onset kidney involvement was emphasised by several Task Force members, because LN represents a major milestone in the natural history of the disease and delaying its diagnosis has profound prognostic repercussions; (3) pursuing a treatment target, which should ideally be remission, as defined by the recent Definition Of Remission In SLE (DORIS) criteria,21 or alternatively, a state of low disease activity, such as the Lupus Low Disease Activity state (LLDAS).22 Both remission and LLDAS have been extensively validated and proven to reduce the risk for damage and other adverse outcomes in patients with SLE (a detailed analysis of the favourable outcomes associated with remission and LLDAS is given in the online supplemental appendix); and (4) the importance of patient adherence to treatment. Specific reference to the issue of adherence in the overarching principles was emphasised by several panellists, including the patient research partners, because medication non-adherence, despite reported wide variations, is considered a major cause of treatment failure.23 A trusting relationship between the physician and patient forms the basis for the minimisation of the risk of non-adherence. 最後の包括的原則はSLEの管理における4つの柱を強調するものである:①早期診断の必要性。その理由は新しく、より感度の高い分類基準の認知が高まっているのにも関わらず最近の研究はSLE患者はいまだに診断の遅れに直面しているからだ(最初の症状から中央値2年)、➁新たな臓器障害、主に腎炎に対する注意深い監視。特に最初の数年。そしてその後も。この新たな腎炎のサインに対する認識の増加の必要性は何人かの委員会メンバーによって強調された。なぜならLNは疾患の自然歴の中で主要なマイルストーンであるため。③治療ターゲット、理想的にはDORIS基準で定められた寛解、あるいはLLDASのような低疾患活動性を目指すこと。寛解、LLDASとも外敵に妥当性が評価されておりダメージと有害なアウトカムのリスクを減らすことが示されている(よいアウトカムの詳細な解析はonline supplemental appendix)。④患者の治療へのアドヒアランスの重要性。包括的原則におけるアドヒアランスの問題に関する特異的な言及は何人かの委員によって強調された;患者の調査パートナーも含まれた。なぜならアドヒアランス不良は報告はまちまちではあるが治療失敗の主な理由と考えられるからだ。医師と患者の信頼関係がアドヒアランス不良のリスクを最小限にするために必要だ。Mean (SD) LoA for the final overarching principle was 9.81 (0.51).
ps;
2023 EULAR recommendations for SLEー個々の推奨1-7ー - リウマチ膠原病のQ&A (hatenablog.com)
2023 EULAR recommendationsー個々の推奨8-12ー - リウマチ膠原病のQ&A (hatenablog.com)